 Kerry Pearl, MS, CCC-SLP, Therapro’s Saturday Seminar speaker on February 11th drew attendees representing a variety of backgrounds who work with children having feeding problems. She spoke about Interventions for Toddlers and School-Age Children with Feeding Difficulties to a rapt audience.
Kerry Pearl, MS, CCC-SLP, Therapro’s Saturday Seminar speaker on February 11th drew attendees representing a variety of backgrounds who work with children having feeding problems. She spoke about Interventions for Toddlers and School-Age Children with Feeding Difficulties to a rapt audience.
Kerry, of Boston Children’s Hospital, specializes in evaluation and treatment of pediatric feeding and swallowing disorders as the Coordinator of the Food School feeding therapy program. Her goal for today’s seminar was to provide information about feeding principles applicable in various settings and how to promote successful oral feeding across disciplines. Kerry has generously made her PowerPoint slides available at this link.
Kerry’s talk covered a lot of ground beginning with the components of the Clinical Feeding Evaluation, which include obtaining the child’s medical history, feeding history, and goals of the caregiver. She stressed that it is important to understand where the child is in terms of his/her skill level and use that as a point of where to begin with treatment for building feeding skills. An interesting thing to consider when evaluating a school-age child, is the importance of exploring what motivates the child…for example, does the child eat their lunch quickly so he/she doesn’t miss recess? Another important factor in evaluation is knowing the child’s eating environment, because it is essential for feeding success. This includes positioning in an appropriate supportive seat that supports the child’s hips, knees, and feet at 90° angles, like a Height Right Chair. When considering the mealtime environment, Kerry advocated establishing a routine so the child knows what to expect, providing clear instructions, and a visual schedule.
Evaluation may identify a number of target areas that need to be prioritized with input from caregivers. Kerry recommended planning intervention in 10 week blocks, which provides time to target several goals and subsequently focus on the skill deficit areas when they become more apparent as treatment sessions progress. Working with the child’s team is important in a number of areas including when it comes to prioritizing what foods to introduce with the child’s dietitian. When initiating therapy, discharge criteria must be in place so that the child’s set, measurable goals can be reviewed to determine whether the therapy has been successful.
A distinctive feature of Kerry’s presentation was her discussion of two intervention models: 1) Operant Conditioning and 2) Sensory Desensitization. She distinguished between the two approaches by discussing how operant conditioning targets behavior directly, is child focused as well as parent focused where the therapist consults with parents to help the parent change the structure of mealtime and nutrition. It involves expanding the foods a child eats, improving volume of intake, and targeting specific behavior or skills. A prompt and immediate reinforcer (like a Wind-Up Toy) is given in treatment so that the eating behavior becomes linked to the prompt and the reward. In this approach, the child builds skills but must overcome their fear associated with eating. Individual therapy is provided and “homework” is given.
In the Sensory Desensitization approach, the child develops skills while gradually adapting, with the focus being on changing mealtime behavior by using modeling and positive reinforcement. In this model, the child progresses through “steps to eating” that include: tolerating the presence of food, interacting with the food, smelling the food, touching the food, tasting the food, and finally eating the food. The end result is that the child experiences less stress around foods and is more willing to try foods. This approach can occur in either individual or group sessions.
When selecting the approach that will be most effective for a particular child, Kerry recommended bearing in mind the child’s current skills and sensory profile as well as family concerns/goals. Considerations should include the child’s nutritional status, oral motor skills, and sensory processing ability.
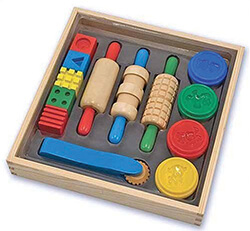
Kerry provided many specific examples of therapeutic activities throughout her talk. Some examples of strategies she discussed to develop chewing skills included lateral placement in the mouth of tools such as the Baby Safe Feeder filled with chewable foods, Chewy Tubes, Y-Chew, or Theratubing dipped in pureed food, progressing to placing small pieces of dissolvable food inside the hollow tubes. Using a Chu Buddy can help the child keep track of the chewy so it is always available.
Kerry’s thoughtful, organized, chock-full presentation provided us with a practical way to approach feeding problems in young children. Her anecdotes, videos, and tidbits of interesting information gleaned from her extensive experience as a feeding specialist complemented her presentation and were greatly appreciated by all who attended her seminar.
As you can see from some the following comments, Kerry’s seminar left attendees with much information and useful treatment strategies:
“The seminar was well organized & relatable. Examples were provided. I enjoyed the contrast of therapy styles & when each were appropriate.” Lauren P., Speech/Language Pathologist
“I would recommend this seminar to a colleague! I loved the specific interventions discussed. I look forward to applying them in my practice.” Marianna Q., Occupational Therapist
“This was a unique learning topic, and I was thrilled for this opportunity to gain more understanding and techniques.” Marisa G., Child Development Specialist
“It was very informative in many ways – I appreciated the intervention strategies given & how they should be implemented. Also, it was helpful to hear how to identify which intervention is best for individual children.”
Amy V., Occupational Therapist
“Very interesting from a teacher’s point of view. It broadened my understanding of the issue & encouraged me to reflect on how the issue can impact classroom learning.” Maura M., Teacher
Thank you, Kerry!
Filomena Connor, MS, OTR/L





 Cathy Collyer, OTR, LMT has treated children with neurological, orthopedic and sensory processing disorders for over 20 years. She is the author of The Practical Guide To Toilet Training Your Child With Low Muscle Tone. Learn more about her work at tranquilbabies.com.
Cathy Collyer, OTR, LMT has treated children with neurological, orthopedic and sensory processing disorders for over 20 years. She is the author of The Practical Guide To Toilet Training Your Child With Low Muscle Tone. Learn more about her work at tranquilbabies.com.
 Kerry Pearl, MS, CCC-SLP, Therapro’s Saturday Seminar speaker on February 11th drew attendees representing a variety of backgrounds who work with children having feeding problems. She spoke about
Kerry Pearl, MS, CCC-SLP, Therapro’s Saturday Seminar speaker on February 11th drew attendees representing a variety of backgrounds who work with children having feeding problems. She spoke about  Evidence based practice (EBP) involves the integration of:
Evidence based practice (EBP) involves the integration of: