Answering the 5 Ws & How
Therapists seeking a practical, evidence-based tool for evaluating children’s functional skills will appreciate the DO-EAT Assessment for evaluating ADLs and IADLs. This unique performance-based assessment is designed to measure how children manage essential Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). By engaging in real-life tasks such as making a sandwich or preparing a drink, children demonstrate their sensory-motor integration, executive functioning, and problem-solving skills. The DO-EAT is a valuable resource for occupational therapists aiming to tailor interventions that promote greater independence and daily success.
What is the DO-EAT Assessment?
The DO-EAT is performance-based; students perform three tasks (making a sandwich, preparing a glass of chocolate milk, and completing a certificate of achievement). These tasks are performed in a sequence one right after the other. Within these three main activities, you have the opportunity to observe the student perform functional tasks that include putting on an apron, setting up the work area, washing their hands, using a knife, following directions, writing, and using scissors. While the student is performing each task you are observing their ability to perform the given task as well as sensory motor skills (like bilateral coordination, fine motor, and posture), performance skills (like attention, organization, and recall), behavioral and emotional components (like motivation and self-efficacy), and the number and types of cues that were given. There is a full description of the DO-EAT on Therapro’s website, DO-EAT-Assessment-Tool-for-Children.html.
What Is & Isn’t Included?
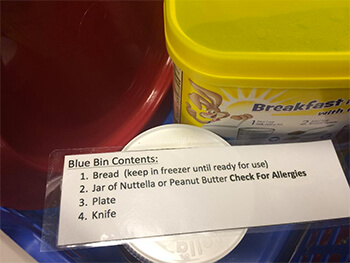
The Do-EAT includes all of the non-perishable materials needed for the assessment, see Therapro’s website for a full list DO-EAT-Assessment-Tool-for-Children.html.
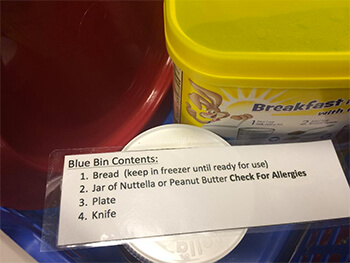
The kit does not include the perishable items (milk, chocolate powder, and sandwich materials). What I have found helpful is to keep a stash of powdered milk and an empty milk jug on hand so that I can make milk when needed. The manual suggests the use of chocolate spread, cream cheese, or hummus for making the sandwich; I usually just keep a jar of Nutella on hand because it has a long shelf life. You will also need bread for the sandwich portion of this; I have access to a freezer so I usually keep a loaf in there but in a pinch I have also asked my very nice cafeteria workers for a slice (for this reason I keep an empty bread bag and clip on hand).
🧑 Who is this Assessment For?
The manual suggests that this assessment is “suitable for children with a chronological or behavioral age of five to eight years old” and that it can be used with children who have a variety of diagnosis including “Developmental Coordination Disorder (DCD), Attention Deficit Hyperactivity Disorder (ADHD), NLD (non-verbal learning disorder) and Learning Disabilities (Rosenblum P.h.D., Josman P.hD., & Goffer M.Sc., 2014)).
I work with high school aged kiddos that have a variety of diagnosis (including autism); all of my students have cognitive delays. The DO-EAT isn’t appropriate for all of my students but I can use it with my students who have the ability to follow basic directives and who have the physical ability to carry out the three tasks involved. When I write my evaluations I make note of the intended ages for this assessment and my justification for using it. There are three defined parts of this test so if I am on the fence about a student’s ability to test I start with the first task and see how it goes from there.
It is important to note that this a very language based test, there are no visuals used and the prescribed dialogue can get heavy. At times, I have found this to be a limiting factor but also a great way to support the need for accommodations including a visual rich environment. For example, I recently did an evaluation with a boy whose primary diagnosis is autism but who also has apraxia and word finding difficulties; he is generally very capable with routine self care tasks (using the bathroom, managing personal hygiene, preparing simple snacks, etc.) however, this was not reflected in the results of the testing due to the breakdown in language skills. With this, I was able to show how important visual supports were to his independence and was able to include that within the accommodations of his IEP.
🗺 Where Can the DO-EAT Assessment be Administered
The manual suggests that this assessment can be performed in a variety of environments. I have only had the opportunity to use it in the school environment (where space is not always easy to come by). I have been able to use it successfully in just about any room I find available as long as there is a table and two chairs. You will also need some sort of shelf/ bookcase/ high spot and a stepstool. Access to a sink is also crucial but it doesn’t have to be in the same room.
⌛ The Big Question on How Much Time?
The manual suggests that this assessment should take about 30 minutes to administer (Rosenblum P.h.D., Josman P.hD., & Goffer M.Sc., 2014); I would agree with that estimate in most cases. It definitely took me longer in the beginning as I was learning the assessment. Scoring on the other hand takes a bit and can be a little tedious; it does get quicker with practice! See below for tips on efficiency.
❔ Why Do I Love the DO-EAT?
The main reason I find the DO-EAT so useful is that it is performance based. As a practitioner I feel I get so much more information when I watch students complete an activity. As OTs we are trained to analyze activities down to the minute detail. With the DO-EAT not only am I able to watch the student perform these activities; the assessment also gives us a structure to analyze the students approach and performance.
❓ How Do I Use the DO-EAT?
I use two main assessments to address ADL and IADL function. Typically I use the PEDI- CAT or The REAL to give me an idea about the specific areas of ADLs or IADLs that a student may be struggling with. From there I use the DO-EAT to answer the “why”.
The observations and analysis of performance skills I gathered while administering the DO-EAT allows me to easily see where a breakdown in a student’s performance is happening (is it an issue with executive function?, is it an issue with decreased fine motor abilities?, etc.) I have a means to connect poor function in a specific ADL or IADL tasks with a cause thus answering the “why”. In addition, the DO-EAT measures the number and types of cues that a student needs in order to perform a task (does a gestural cue work?, can they figure it out with an indirect verbal prompt?, do they need a direct verbal cue?). With this information my evaluations and eventual goal writing become focused; in addition I now have a baseline.
💡 Other Information & Helpful Tips
- There is a parent questionnaire used as part of this assessment. The parent questionnaire is great in that it gives you a better understanding of the student’s function in environments that you may not necessarily be able to observe. What I appreciate, however, is that those responses are not needed to score the evaluation (in my experience, not every questionnaire that gets sent home comes back!).
- I would recommend practicing this assessment on a colleague/ friend/ spouse/ etc. before using it functionally. There is quite a bit involved with the observation piece of it.
- The manual describes the setup very well; I have that page marked so that I can “check off” each piece as I go.
- I put cards in each of my baskets so that the set up is easy and mindless.
- When learning this assessment, I found it extremely helpful to record the student completing the assessment (I just took a quick video using my phone). There are a lot of details to observe; I found it overwhelming to simultaneously administer the test and also complete the observation checklist. I was able to get much more information by recording my sessions and then completing the scoring later while watching the video.
Works Cited
Rosenblum P.h.D., S., Josman P.hD., N., & Goffer M.Sc., A. (2014). DO-EAT Performance Based Assessment Tool for Children: Manual. (J. Hahn-Markowitz, M.Sc., Ed., & S. Veeder, Trans.) Wayne, NJ, USA: Maddak Inc.
Allyson Locke, MS, OTR/L
 Allyson is an occupational therapist with a diverse background in both sensory integration and school based practice. She currently works in a school for children and young adults who have significant medical, mental health, and cognitive needs.
Allyson is an occupational therapist with a diverse background in both sensory integration and school based practice. She currently works in a school for children and young adults who have significant medical, mental health, and cognitive needs.




 Allyson is an occupational therapist with a diverse background in both sensory integration and school based practice. She currently works in a school for children and young adults who have significant medical, mental health, and cognitive needs.
Allyson is an occupational therapist with a diverse background in both sensory integration and school based practice. She currently works in a school for children and young adults who have significant medical, mental health, and cognitive needs.




 Cathy Collyer, OTR, LMT has treated children with neurological, orthopedic and sensory processing disorders for over 20 years. She is the author of The Practical Guide To Toilet Training Your Child With Low Muscle Tone.
Cathy Collyer, OTR, LMT has treated children with neurological, orthopedic and sensory processing disorders for over 20 years. She is the author of The Practical Guide To Toilet Training Your Child With Low Muscle Tone.