Occupational therapy (OT) plays a vital role in promoting a healthy lifestyle by supporting physical, mental, and emotional well-being. From physical activity and sensory regulation to healthy eating habits and stress management, OTs empower individuals to build routines that enhance their overall health.
This Occupational Therapy Month, let’s explore key strategies OTs use to promote healthy lifestyles and share resources to support therapists in their work.
1. Promoting Healthy Lifestyles with Physical Activity & Movement 🚶♂️💪
Regular movement is essential for strength, coordination, balance, and overall well-being. Occupational therapists encourage fun, engaging activities that promote motor skills and physical fitness in both children and adults.
Therapro’s Top Picks for Movement & Mobility:
🔹 Wobble Chairs & Stability Discs – Great for improving core strength and active sitting in classrooms and therapy sessions.
🔹 Balance Boards & Stepping Stones – Help with coordination, balance, and motor planning while keeping movement engaging.
🔹 Therapy Balls – Ideal for vestibular input and postural control exercises.
🔹Resistance Bands – Fun ways to develop upper body strength, endurance, and proprioceptive input.
🔹 Browse more movement tools here: Therapro’s Move-To-Learn Collection
💡 Therapist Tip: Incorporate movement breaks throughout the day to help children and adults maintain focus, regulate energy levels, and reduce stress.



2. Promoting Healthy Lifestyles with Sensory Regulation & Mindfulness 🧘♀️
Managing sensory input and practicing mindfulness are essential for reducing stress and supporting mental well-being. OTs use sensory-friendly activities to help individuals stay calm, focused, and self-regulated throughout the day.
Therapro’s Top Picks for Sensory Support:
🔹 Fidget Tools – Support focus and self-regulation with tools like Therapro’s Fidget Kit and Koosh Ball Fidgets.
🔹 Weighted Products – Deep pressure input from Weighted Blankets, Compression Vests, and Shoulder Wraps can provide a calming effect.
🔹 Chews & Oral Motor Tools – Items like Chewable Jewelry and Bite-N-Chew Tips help with oral sensory needs and self-soothing.
🔹 Sensory Seating – Products like the Disc ‘O’ Sit Cushion promote active sitting while offering subtle movement input.
🔹 Therapeutic Brushes & Tactile Sensory Items – The Wilbarger Therapressure Brush supports sensory defensiveness, while Cuddle Balls provide rich tactile input.
🔹 Explore more sensory tools here: Therapro’s Sensory Collection
💡 Therapist Tip: Create a sensory toolkit for home, school, or therapy sessions, including fidgets, weighted tools, and calming visuals to support self-regulation throughout the day.



3. Promoting Healthy Lifestyles with Healthy Eating Habits & Self-Care 🍎🥗
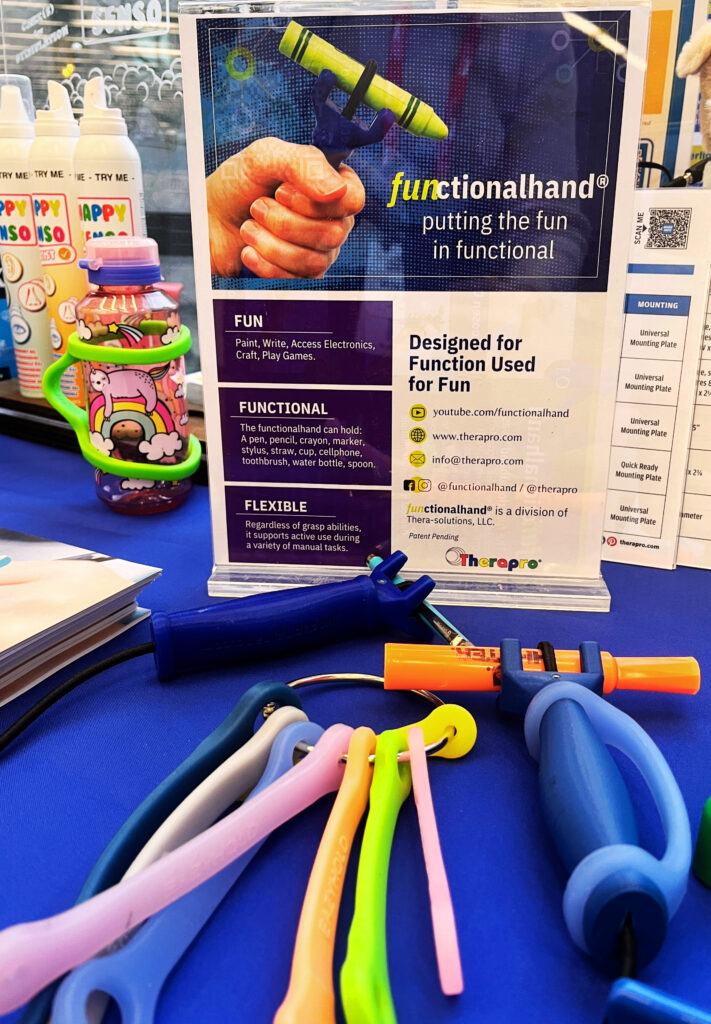
Nutrition and self-care routines are essential parts of a balanced lifestyle. OTs help individuals with feeding challenges, adaptive utensils, and personal care skills to promote independence in daily routines.
Therapro’s Top Picks for Mealtime & Self-Care:
🔹 Adaptive Utensils & Cups – Products like the TheraBear Drinking Cup and Maroon Spoons support individuals with oral motor and self-feeding challenges.
🔹 Plate Guards & Non-Slip Placemats – Tools such as the Inner Lip Plate and Dycem Mats help prevent spills and encourage independent eating.
🔹 Visual Schedules & Timers – Supports like the Time Timer can help establish structured mealtime and self-care routines.
🔹 Dressing & Grooming Aids – Items like Button Hooks, Shoehorns, and Zipper Pulls assist with developing dressing independence.
🔹 Oral Motor Tools – Whistles, straws, and chew tools aid in strengthening oral muscles for feeding and speech development.
🔹 Explore more daily living tools here: Therapro’s Daily Living Collection
💡 Therapist Tip: Encourage families to set up predictable daily routines using visual schedules, timers, and adaptive tools to promote independence and reduce stress.



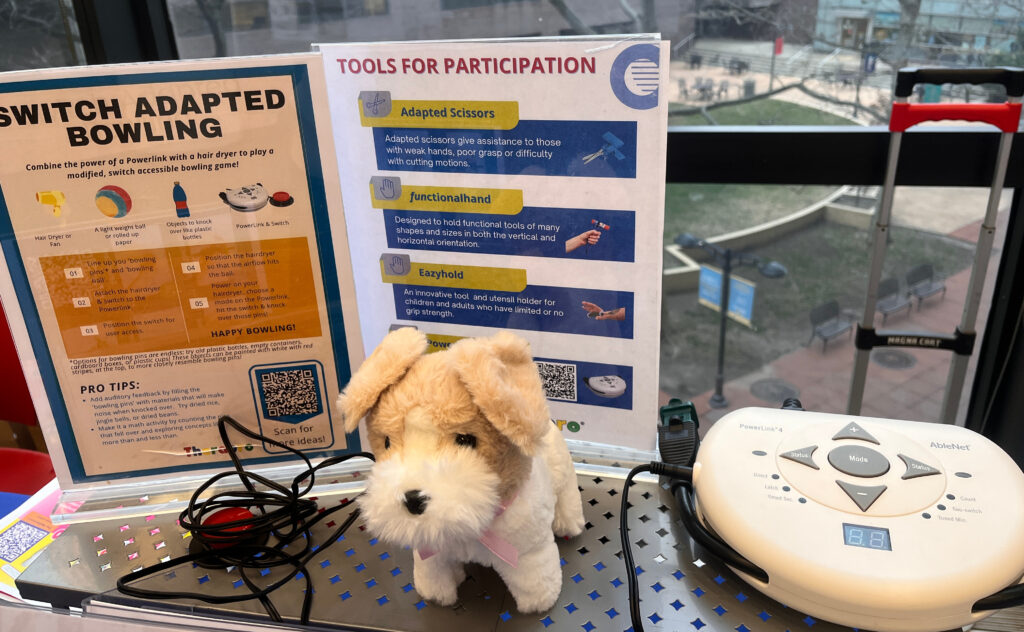
4. Promoting Healthy Lifestyles with Social Participation & Mental Health 🤝💬
A healthy lifestyle includes building meaningful relationships, developing social-emotional skills, and managing emotions effectively. OTs support clients in fostering social communication, emotional regulation, and self-awareness to promote overall well-being.
Therapro’s Top Picks for Social-Emotional Learning (SEL):
🔹Social Awareness & Conversation Tools – Games like Let’s Talk Cubes and Webber® Photo Cards – What Are They Thinking? encourage turn-taking, perspective-taking, and conversation-building.
🔹 Coping & Self-Regulation Tools – The Big Feelings Pineapple and My Spark Cards Tool Box teach essential strategies for stress management and emotional resilience.
🔹 Explore more SEL resources here: Therapro’s Social-Emotional Learning Collection
💡 Therapist Tip: Use visual supports, role-playing, and structured social games to reinforce emotional regulation, problem-solving, and positive interactions in therapy sessions.
Join the Conversation! 🗣
💡 What are your favorite OT strategies for promoting healthy lifestyles? Tag @Therapro in your social media posts!
Let’s work together to empower individuals to move, learn, and live well every day!