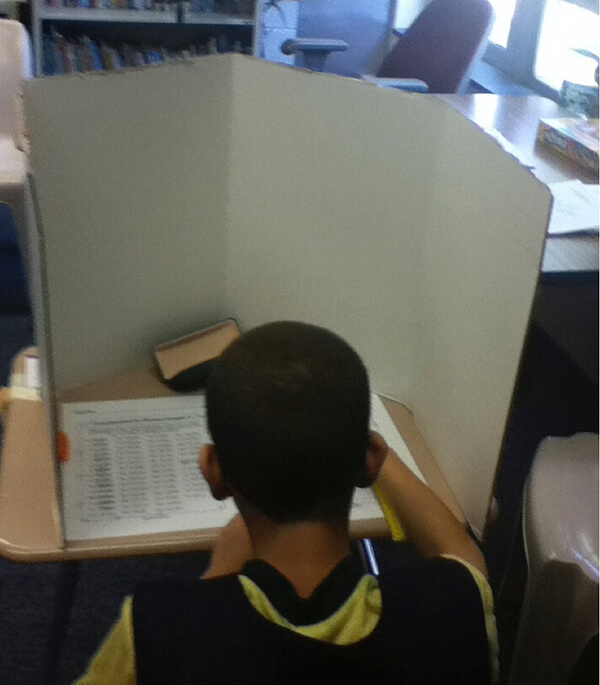
Over responsive sensory systems need opportunities to take breaks from sensory stimuli through the day. The analogy of a Thanksgiving feast can be used to illustrate an over responsive sensory system. After a large Thanksgiving meal we may get to the point where we simply can not add another bite of food to our very full bellies, doing so would just make us sick. The over responsive sensory systems are filled to capacity with sensory stimuli and can not handle another bit of sensory information. When the sensory system hits capacity you may see things like big reactions to small problems or ‘shut down’ types of behavior. Just like a nap after a Thanksgiving meal does wonders to help digest and reset our full bellies, a break from sensory stimuli does wonders for the over responsive sensory systems. Total elimination of sensory stimuli is nearly impossible but offering a space with dampened sensory stimuli, to retreat to when needed, can help with overall regulation through the day, leading to greater ability to successfully participate and attend. These spaces can often be created with minimal equipment and little space. Check out these ideas:
Cozy Corners: Corners are a great spot to set up a calming space; corners naturally provide barriers on two sides and are a great spot to tack a small blanket overhead to create a roof. These types of spaces are especially great for sensory systems that are easily overwhelmed by tactile input. The walls provide a barrier from unwanted tactile sensations like the accidental bump from another child or the breeze from a fan.
Forts. Forts can be created by simply throwing a blanket over a table or two opposing chairs. Forts are great for sensory systems that are easily overstimulated by visual input because forts are dark and act to eliminate extraneous visual input.
Retreat Space. Occasionally we are lucky to find an unused space away from the hustle and bustle of daily life. This may be an outdoor area, an accessible attic or basement space, or a nook in the corner of a porch. These types of spaces are ideal for sensory systems who have difficulty filtering out extraneous auditory or olfactory stimuli (so important to consider as we get into the holidays and all the cooking that comes along with it).
The availability of these spaces is often enough to help the overstimulated sensory system regroup and decompress. However, additions to these spaces may be helpful! Some ideas include:
- Beanbags. Beanbags are a great way to increase deep pressure input to help organize and regulate an over stimulated sensory system. The High Back Bean Bag Chair is a great option when more support is needed. The HowdaHUGS chair is a great option for smaller spaces or when portability is needed (take it on that trip to grandmas along with a small blanket for an instant retreat space during the holiday hustle and bustle)!
- Noise Cancelling Headphones. Headphones help filter out extraneous auditory input allowing the other sensory systems a chance to regroup!
- Weighted Items. Weighted items, when used appropriately, can be a great source for deep pressure input that helps to organize an over stimulated sensory system. There are so many to choose from; weighted lap pads, weighted animals, and shoulder wraps.
- Oral Input. Resistive sucking using a water bottle or through a straw, blowing bubbles, or using a chew all are great ways to provide organizing proprioceptive input.
The availability of a space that limits extraneous sensory stimuli can be a welcome relief for those struggling with over responsive sensory systems. Having access to a place that allows the sensory systems to regroup, decompress and re-organizes can lead to greater participation in day to day activities. These spaces can easily be created with everyday items found around the home!




 The Therapro exhibit was constantly buzzing with attendees searching for the best tools for their school-based practice. Ginger MacDonald, OTR/L, co-author of
The Therapro exhibit was constantly buzzing with attendees searching for the best tools for their school-based practice. Ginger MacDonald, OTR/L, co-author of