With academic demands increasing in the school setting, students’ free time is decreasing, and teachers try to create activities and stations for children to practice specific academic skills during class time. Occupational therapy practitioners have expertise in enhancing learning with fine motor tools, creating innovative interventions that combine fine motor development activities with academic skill development.
Here is a list of some simple fine motor activity ideas that can be used to support academic learning within the classroom environment. If you get creative you can come up with several ways to mix and match items to multiply the possibilities. Remember to share with your teachers.
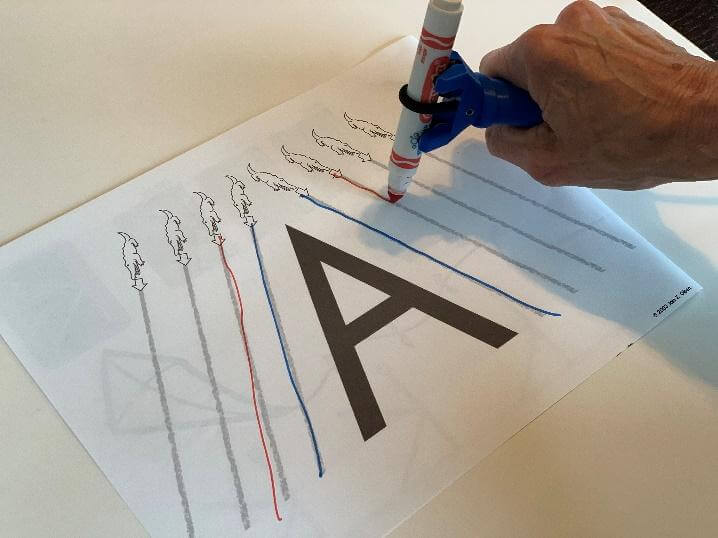
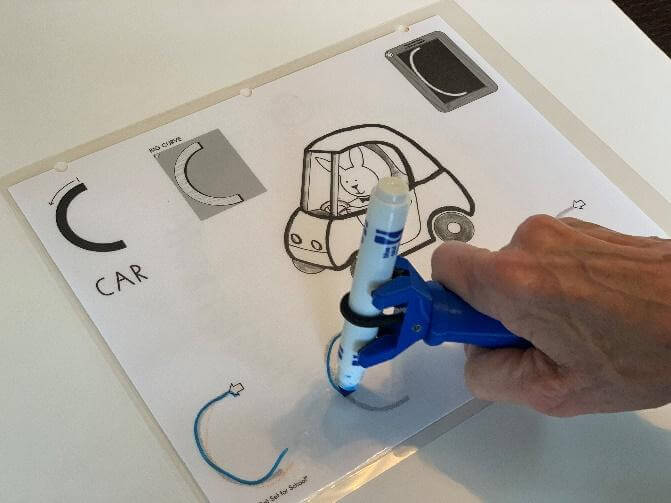
1. Letter Names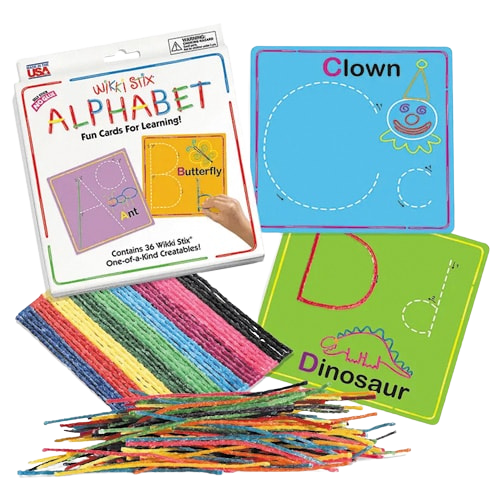
- Playdoh letter formation
- Cryptograms
- Wikki Stix
- Stickers
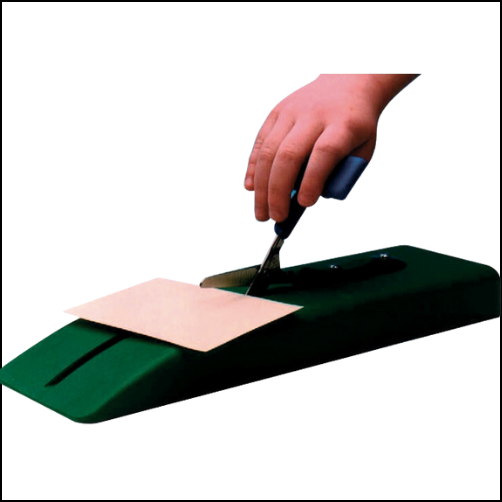
- Hole punching letters
- Matching on cards using clothespins
- Letter tiles to match words
- Alphabet Stamps
- Letter beads on pipe cleaners
- Stacking Legos, Blocks, Unifix cubes with letters on it to make words
- Catching and spelling letters
- Velcro letters
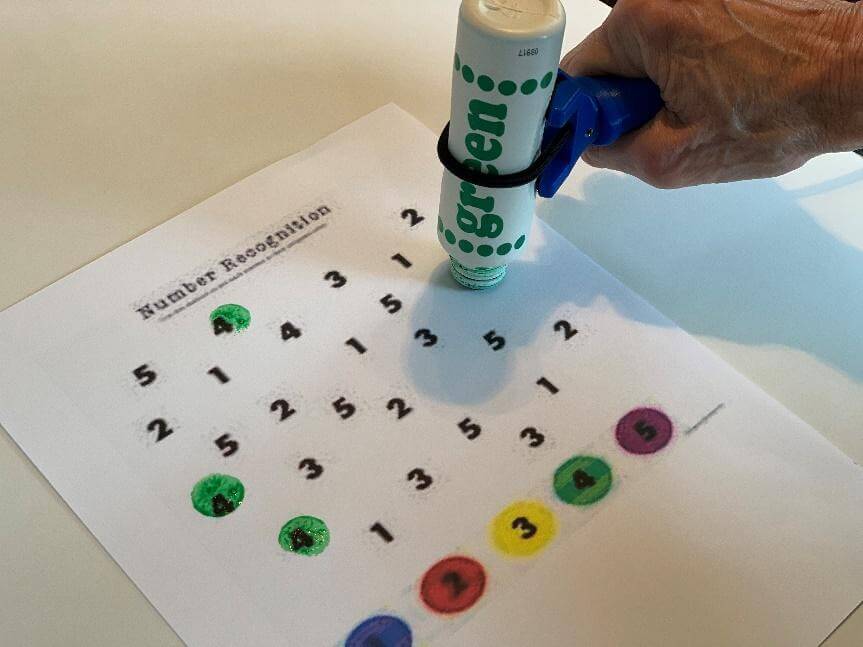
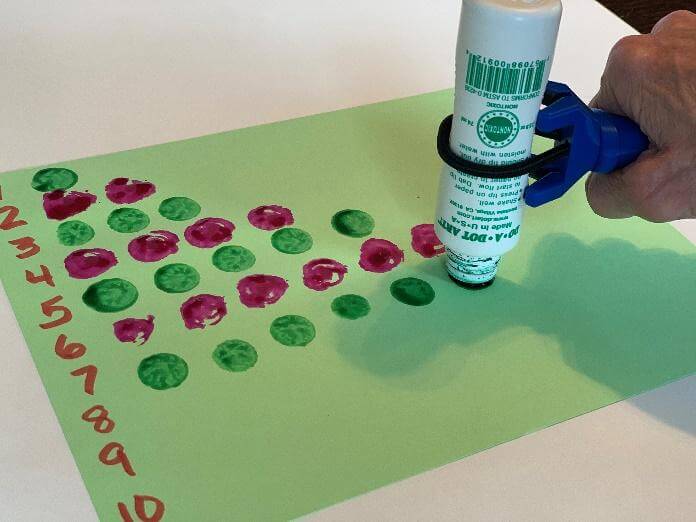
- Using tongs to count items and match to a number
- Dice games
- Using a sand tray to write numbers
- Puzzles
- Searching for items in rice bin and match to number cards
- Making math equations with beads on pipe cleaners
- Creating a 10 frame out of egg carton
- Stacking blocks to create patterns
- Putting counters into slotted containers
BONUS!
Adapting many of these to remote learning is pretty easy. You can even host a scavenger hunt for the students to search their house to gather materials to create kits
The options for integrating fine motor tools into learning is limitless. I’m hoping I’ve listed a new one here for you to try with your students.
Guest Blogger: Moira P. Bushell OTD, MEd, OTR/L