A physical therapist called me from Ohio wanting to know more about the S’Cool Moves products, but what she really needed from me were some insights that I’ve gained from doing what I do for the last twenty years. She was a therapist making the huge shift from clinical practice to educational practice in schools. She told me that she was the ONLY physical therapist for the entire district and was spread really thin. Let’s call our therapist Amber. Amber said that the teachers seemed to want to know what they could do in the classrooms for all the students to improve foundation skills. But how was she going to reach all these teachers and satisfy the IEP goals for her huge caseload?
It was interesting. Do you know where my mind went to help Amber create a framework? It went to sharing about the Response-to-Intervention model (RTI). RTI was designed as an alternative to the discrepancy model used to determine if a child qualified for special education services. With RTI, methods of intervention are validated and data collected prior to referring a child for special education testing. Though some report RTI working well, for others it’s a mixed bag depending on how it is being implemented.
What if we could use RTI personally? Let’s call it the RTI-P model. During our conversation, I found myself explaining to Amber how RTI models work and personalizing the model for her. She got off the call with clarity and new tools to help guide her as she navigates her new position.
Today’s thought is, “How can we use RTI-P to organize our jobs and therapy caseloads?” Think in terms of tiers. RTI has three tiers. The first tier includes interventions and strategies we can use with all students in the classroom. The second tier includes modifications we need to make for small groups of students who are having difficulty with the class-wide strategies. The third tier focuses on individual strategies for the most involved students.
In your caseload, what students do you have that you could support in the classroom setting, Tier 1? Are there opportunities for you to present some strategies during staff meetings or on PD days to support teachers and students in the classroom?
Now think about Tier 2. What students need small group support either in the classroom or within designated smaller group environments?
And finally, Tier 3. What students are very involved and need your one-on-one, hands-on support?
Once you create your own personal framework, then you can figure out what materials or products will help you reach your goals, but first create your RTI-P framework.
For instance, Therapro’s Drive Thru Menus works well with all student in a classroom so this could be considered as an important tool for Tier 1 intervention. For small groups of students who are working on improving visual-motor integration, consider
- Origami Fun for Beginners – 55 fun-to-do projects! Includes 96 sheets of authentic origami paper in a gorgeous array of colors and designs.
- Letter Treasure Hunt Game – Handwriting fun!
- Sail your ship to an Alphabet Island,
- Follow Captain’s orders when you draw a card,
- Collect your treasure by writing the letter in the Captain’s log.
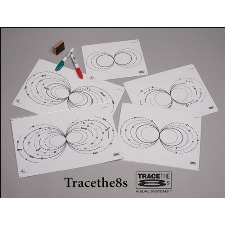
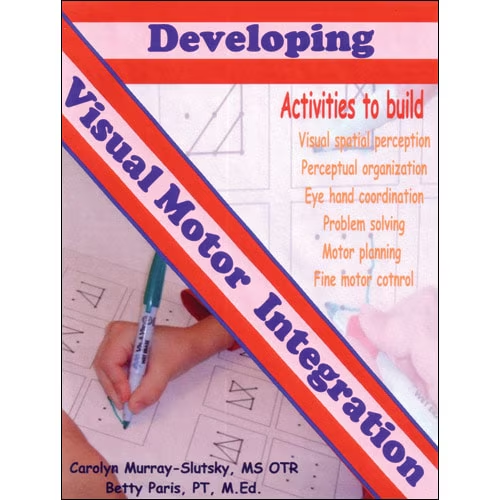
For students needing one-on-on intervention, add Developing Visual Motor Integration and Trace the Eights to your intervention strategies.

Let me know if the RTI-P makes sense to you and how you’ve used it to be more effective in your job and less stressed!
Thanks for all you do for children, Dr. Debra Em Wilson
Guest Blogger: Dr. Debra Em Wilson. I’m excited to join Therapro as a guest blogger. I am a reading specialist and the founder of S’cool Moves. I enjoy collaborating and appreciate this opportunity to connect with the Therapro community.