The 2017 ASHA conference drew over 14,000 speech-language pathologists, audiologists, hearing and speech scientists, and communication sciences and disorders students to Los Angeles for three jam-packed days of educational, networking, and fun events. On Thursday we welcomed the masses into the Expo Hall when they stopped by the Therapro exhibit by asking attendees what parts of the opening session inspired them. They reported enjoying Goldie Hawn’s Keynote Address with her emphasis on mindfulness and self-regulation. She discussed her foundation, the Hawn Foundation, which focuses on a program for schools to teach children the basics of brain science. It was a great kick-off for this year’s conference. Read on for more conference highlights!
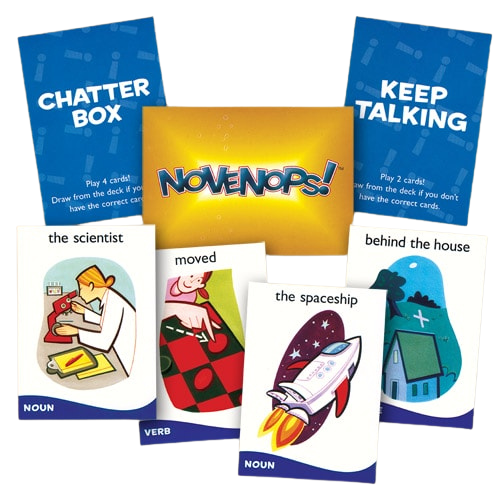
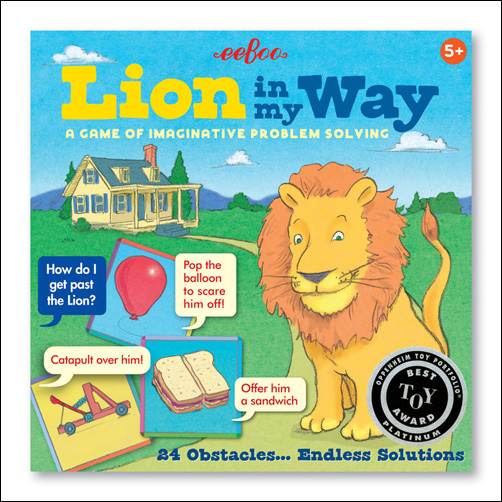
We designed our exhibit this year to focus on various areas we thought would interest attendees. Our “Games Corner” was a beehive of activity with Karen drawing therapists to play Novenops, Trunks, Letter Treasure Hunt, A Fistful of Coins, and Obstacles: A Game of Imaginative Solutions. One therapist loved Novenops so much that she purchased one for herself and several for gifts! The zany sentences players constructed in this game had everyone laughing.

Another area we set up was filled with wind-up toys that drew a crowd with giggles, exclamations, and stories of creative ways they used the toys in therapy sessions. Everyone exclaimed how unique our collection was, including the Firefighter, Cats, Lovely Farm, Baby Critters, and retro appliances.
Friends we had met in previous years stopped by to say hello and to see what’s new at Therapro. Our auditory processing publications were much appreciated, including Help for Auditory Processing and The Source for Processing Disorders – 2nd Edition. Story Starters Write-Abouts and Silly Starter Write-Abouts were very popular flip books with which students gain valuable writing and expressive verbal practice. Therapists loved the Conversacards, Question Series and Question Set with beautiful photos on one side and easy teaching steps on the reverse side.
Therapists who address feeding problems were excited to meet Kelly VahnDam, MS, CCC-SLP, editor and an author of the Therapro publication Pediatric Feeding Disorders. She graciously autographed the book and took photos with admirers. Several students from North Carolina reported that her book is part of their curriculum. Feeding therapists picked up Textured Spoons, Nuk Massager Brushes, Mr. Juice Bear, and much more. It was fun to help therapists select appropriate materials and brain storm with them on ways to use chewies for their clients. Mary Schiavoni, MS, CCC-SLP, creator of Chewy Tubes visited our booth and introduced the new Sensory Dipper she showcased at the conference. Dawn Winkelmann, MS, CCC-SLP of ezpz stopped by as well – we love their Happy Mats and Happy Bowls!
After three exciting and full days of introducing Therapro to speech and language professionals from the US, Canada, and many foreign countries, we were pleased with the dedication and thirst for knowledge expressed by those we met. We left L.A. satisfied that we had met thousands of devoted and gifted therapists who truly LOVE their profession!
We can’t wait to welcome you to Boston next Fall for the ASHA Conference 2018!
Filomena Connor, MS, OTR/L

 Kerry Pearl, MS, CCC-SLP, Therapro’s Saturday Seminar speaker on February 11th drew attendees representing a variety of backgrounds who work with children having feeding problems. She spoke about
Kerry Pearl, MS, CCC-SLP, Therapro’s Saturday Seminar speaker on February 11th drew attendees representing a variety of backgrounds who work with children having feeding problems. She spoke about