It seems as natural as can be; use a child’s meals and snack times as opportunities for teaching utensil use. In this atmosphere of “least restrictive environment” and push-in treatment, this sounds like a great plan for your therapy session. Although it seems like a good idea, there are circumstances in which separating utensils beyond mealtime, at least initially, can be more effective in treatment:
- Children with tactile aversions and oral sensitivity may find combining manual and intra-oral exploration to be too overwhelming.
- Children with both motor and sensory issues may find that they cannot work on practicing multiple skills at the same time.
- Children with behavior issues can be faced with a difficult situation: they want to eat and they want to exert control over their body or an adult’s behavior.
- Kids with minimal endurance or tolerance can lack the ability to complete a meal, leaving them dependent on adults or frustrated with their fatigue or a sense of failure.
Teaching utensil use without the expectation of food ingestion can solve these problems. As skills and tolerance grow, the two experiences can be joined successfully. Here are some suggestions to make practice effective and weave it back into functional experience as seamlessly as possible:
- Have the child feed an adult using child-friendly utensils and foods. A child may decide to take a bite instead of feeding the adult, so a food’s size and texture should be safe for the child’s developmental level.



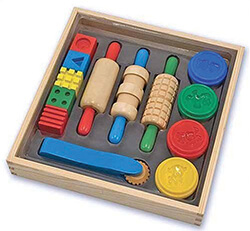
- Playfully scooping and piercing non-food objects such as non-edible dough with utensils and other “real” tableware may extend practice sessions while decreasing the stress of multi-sensory exposure with food.


- Watching the therapist eat food that the child has prepared or served with utensils reinforces the social and nurturing aspects of meal preparation and eating.
- Using strategies such as backward chaining or graded exposure, activities that begin by separating utensil use from eating can become more like a typical mealtime experience over time. When children are given a “just-right” level of challenge, they make faster progress with ease.
Cathy Collyer, OTR, LMT, PLLC
 Cathy Collyer, OTR, LMT has treated children with neurological, orthopedic and sensory processing disorders for over 20 years. She is the author of The Practical Guide To Toilet Training Your Child With Low Muscle Tone.
Cathy Collyer, OTR, LMT has treated children with neurological, orthopedic and sensory processing disorders for over 20 years. She is the author of The Practical Guide To Toilet Training Your Child With Low Muscle Tone.

 Evidence-based practice (EBP) involves the integration of:
Evidence-based practice (EBP) involves the integration of: