Games are a useful therapeutic tool; they are versatile, engaging, and so much fun! WIth a few simple modifications games can address a wide range of therapeutic needs. A few simple modifications can be used for almost every game:
- Add Visuals. Visuals can be anything from simplified directions to communication aids, like “your turn” and “my turn”. Visuals can help those who struggle with sequencing, memory, or communication participate more independently in game play.
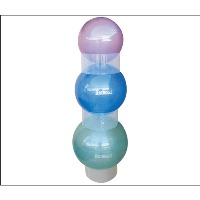
- Change the playing position. Playing games on the floor, at a countertop, or with alternative seating helps to increase participation and access. Playing a game on the floor allows players to play in alternative positions, like laying on their bellies. This position is great for those with postural instability, and helps increase their focus and endurance. Another option is to use a therapy ball (add a base for stability), Alert Seat, Ball Chair, or air filled cushion instead of a traditional chair. These types of alternative seating provides movement input which may allow those with shortened attention spans to participate longer and with more focus. Some games like, Left Center Right, have few manipulatives making these great games to use on scooter boards or swings.
- Modify the Manipulatives. Some game pieces are just too small, too big, or too difficult for students to access. One quick fix is to swap out the game tokens for something more manageable like a jumbo dice. Another option, insert game pieces into putty for a bigger gripping surface. Other modifications include using a card holder or book holder.
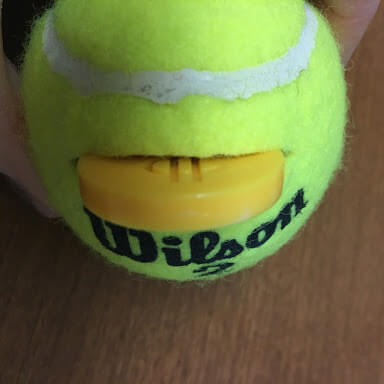
- Manipulating the manipulatives to target hand skills. To encourage a pincer grasp, place smaller game pieces into an egg carton (or similar small container); the smaller space allows for only a few fingers to access the piece, encouraging a two or three finger grasp pattern every time the player picks up the game pieces. To incorporate hand strengthening and bilateral coordination, use a tennis ball with a small slit cut into it. Players must squeeze the tennis ball with one hand while using the other hand to insert or remove their pieces. To target fine motor manipulation with insertion, use plastic containers (your recycling bin is a great resource); cut a slit in the lid and work on inserting game manipulatives into the containers.
- Change the game rules to address specific therapeutic goals. If your focus is social interactions, team building, or cooperative problem solving, change game play so players play as a group instead of competing against each other. If you are doing individual treatment sessions instead of group sessions, change gameplay to make it a single-person game. When time is limited or you have participants who struggle with extended attention and focus, add a time rule where gameplay ends after a set amount of minutes. When the game is too hard or too easy for players, add more complexity or decrease the complexity.



With a little bit of creativity, most games can be changed, adapted, or modified in order to use them as a therapeutic tool. Check out Therapro’s handy games guide to see these modifications applied to some of our great games!




 Occupational Therapist, healing facilitator, certified infant massage instructor, freelance writer, author of
Occupational Therapist, healing facilitator, certified infant massage instructor, freelance writer, author of