Pediatric Feeding Disorder (PFD) presents significant challenges for children and their
families; raising awareness about PFD is crucial for early diagnosis and intervention, ensuring that children receive the appropriate care and support. This disorder can affect a child’s ability to eat and drink, impacting their nutrition, growth, and overall development. It is defined as “impaired oral intake that is not age-appropriate, associated with medical, nutritional, feeding skill, and/or psychosocial dysfunction.” Studies show that in the United States, PFD affects more than 1 in 37 children under the age of 5. The American Occupational Therapy Association (AOTA) and Feeding Matters have been at the forefront of these efforts, working collaboratively to enhance understanding and recognition of PFD.
Understanding Pediatric Feeding Disorder
Pediatric feeding disorders encompass a broad range of difficulties related to eating and
drinking. These can include medical, nutritional, feeding skill-based, and psychosocial
aspects. Common symptoms may include difficulty with sucking, chewing, or
swallowing, aversion to certain textures or foods, and disruptive mealtime behaviors.
Early identification and intervention are essential to prevent long-term consequences,
such as malnutrition, growth delays, and social-emotional issues.
The Role of AOTA in Addressing Pediatric Feeding Disorder
The American Occupational Therapy Association (AOTA) plays a vital role in promoting
the role of occupational therapy in the assessment and treatment of Pediatric Feeding Disorder. Occupational therapists are uniquely equipped to address the complex interplay of physical, sensory, and psychosocial factors involved in feeding disorders. Through education, advocacy, and research, AOTA supports occupational therapists in providing evidence-based interventions to improve feeding outcomes for children.
Key Initiatives by AOTA:
- Educational Resources: AOTA offers comprehensive resources and continuing education opportunities for occupational therapists to stay updated on the latest research and best practices in pediatric feeding.
- Advocacy: AOTA advocates for policies and practices that support early identification and intervention for PFD, emphasizing the importance of interdisciplinary collaboration.
- Research: AOTA promotes research in the field of pediatric feeding, encouraging the development of innovative assessment tools and intervention strategies.
Feeding Matters: A Leading Voice in Pediatric Feeding Disorder Advocacy
Feeding Matters is a nonprofit organization dedicated to advancing the understanding
and treatment of pediatric feeding disorders. Founded by parents of children with PFDs
Feeding Matters aims to provide support, education, and resources to families and
professionals alike. The organization works tirelessly to create a world where children
with feeding disorders thrive.
Key Contributions by Feeding Matters:
- Educational Programs: Feeding Matters offers a range of educational programs for parents, caregivers, and healthcare professionals to increase awareness and understanding of PFD.
- Support Networks: The organization provides support groups and resources for families, fostering a sense of community and shared experiences.
- Research and Advocacy: Feeding Matters collaborates with researchers and advocates for policy changes to improve the diagnosis and treatment of PFD. For example, they have worked effectively to develop the Feeding Matters Infant and Child Feeding Questionnaire (ICFQ) – an age-specific tool designed to identify potential feeding concerns and facilitate discussion among the child’s healthcare team. It was designed by a group of internationally esteemed contributing authors including occupational therapists, speech-language pathologists, physicians, dietitians, and more.
Collaborative Efforts: AOTA and Feeding Matters
The collaboration between AOTA and Feeding Matters has been instrumental in raising
awareness and improving the diagnosis and treatment of PFD. By combining the
expertise and resources of both organizations, they have made significant strides in
addressing the challenges faced by children with feeding disorders.
Joint Initiatives:
- Public Awareness Campaigns: AOTA and Feeding Matters have launched joint campaigns to educate the public and healthcare professionals about the signs and symptoms of PFD, emphasizing the importance of early intervention.
- Interdisciplinary Conferences: Both organizations co-host conferences and workshops that bring together experts from various fields, including occupational therapy, speech-language pathology, nutrition, and psychology, to share knowledge and best practices.
- Research Collaboration: AOTA and Feeding Matters support and fund research projects aimed at developing innovative approaches to the assessment and treatment of PFD.
The collaborative efforts of AOTA and Feeding Matters have significantly advanced the awareness, diagnosis, and treatment of pediatric feeding disorders. By promoting education, advocacy, and research, these organizations ensure that children with PFD receive the comprehensive care they need to thrive. Continued collaboration and support from the broader healthcare community are essential to furthering these efforts and improving outcomes for children and families affected by feeding disorders.
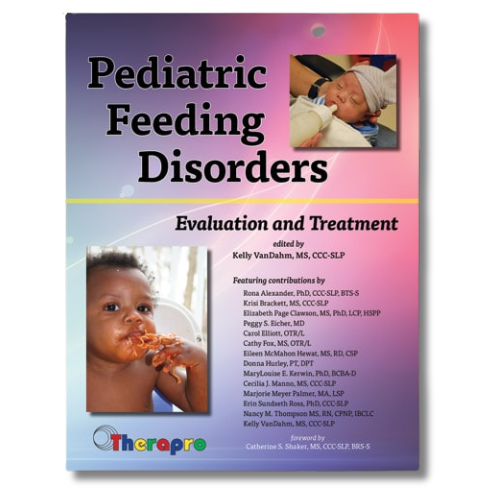
Check out these important feeding resources that Therapro offers for your personal
library.
Gust Blogger: Filomena Connor, MSOT – Retired












